Collegiate Recovery Program
The Collegiate Recovery Program (CRP) at Kennesaw State University is your dedicated
resource for offering a supportive and thriving recovery community on campus. Our
CRP is designed to provide a safe and inclusive space where students in recovery can
find the resources, connections and guidance they need to excel academically and maintain
their sobriety at KSU and beyond. Whether you're a current student in recovery or
interested in learning more about our program, get more information about upcoming
events and support services tailored to your unique journey.
Discover how CRP can enhance your college experience and empower you to achieve your
academic and personal goals while embracing a life of recovery.
Learn More
|
Recovery Support for Students
The Recovery Support Services at Kennesaw State is your go-to resource for programs
and services designed to support your journey to recovery and well-being. At KSU,
we understand the importance of maintaining a healthy and balanced lifestyle while
pursuing your academic goals. Here, we hope to provide you with access to a comprehensive
set of resources, from counseling and peer support to educational workshops and events,
all aimed at helping you thrive in your time here at Kennesaw State.
Explore these offerings and discover how our university is committed to providing
you with the support you need to succeed academically and personally, while embracing
a life of wellness and recovery.
Learn More
|
|
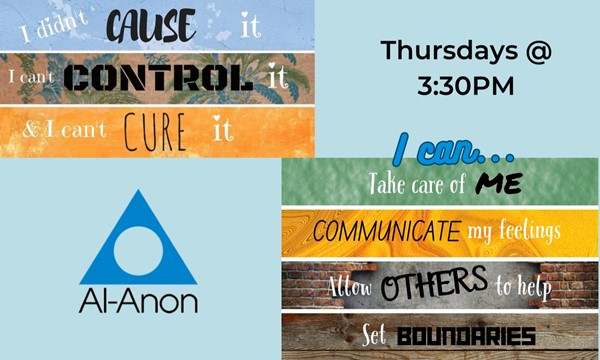
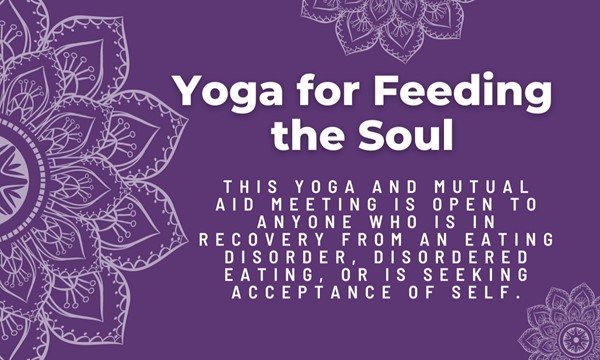
Get familiar with the events and programs happening throughout the year at Kennesaw
State University's Center for Young Adult Addiction and Recovery (CYAAR). Stay informed
with the latest events, workshops and activities that CYAAR offers to support your
personal, professional and academic goal towards complete wellness. Our events are
thoughtfully created to provide you with opportunities for growth, connection and
education.
Get involved with a variety of campus programs and join us at our upcoming events
to experience the benefits of a vibrant, recovery-focused community right here at
KSU.
Learn More
|
Alcohol and Other Drug Educational Resources
The Office of National Drug Control Policy reports that a quarter of college students
face negative academic consequences due to drinking, such as missing classes, falling
behind, and lower grades. Substance use on campus poses significant risks, from academics
to health and safety. At Kennesaw State, our approach focuses on two key elements:
- providing recovery-informed education to college students and
- advocating for cultural changes in substance use norms.
We emphasize peer-to-peer educational models, effectively engaging students in reevaluating
their perceptions of substance use to promote a healthier campus culture. Get more
information on alcohol and drug resources available to all KSU students!
Lear More
|
Recovery Science Research
The Recovery Science Research Collaborative (RSRC) hosted by Kennesaw State brings
together researchers and practitioners to advance the science of recovery. At RSRC,
professionals, students, and stakeholders from various backgrounds collaborate to
explore the theoretical foundations of recovery science, develop meaningful measures
of individual and community recovery, and share their discoveries to influence recovery-related
policies and practices.
Learn more about this collaborative effort that fosters a think-tank-style environment
and empowers recovery researchers and practitioners to collectively propel the field
forward.
Learn More
|
|